Stress is a part of everyday life, it is necessary to give us the drive we need to get things done.
However, when it comes to chronic stress, this is something that we have come all to familiar with as a part of a normal way of being.
Stress is defined as a strain or overexertion on our bodies, and our minds.
It is associated with feelings and actions we all know too well, the overwhelm, sleepless nights, excessive thinking, emotional releasing, outbursts, anger, frustration, helplessness, constant worry, nausea, panic and uncontrollable crying.
While these are all outward expressions of stress, it is also relevant to address the internalisations of it as well, for those whom tend to keep the feelings bottled up inside and perhaps not to show a physical exertion, and yet are just as effected by the underlying health issues this can have on the mind and body.
Stress has a huge impact on our physical and emotional body. It effects our gut flora and in turn therefore effects our mental well-being.
The microbiota in our guts are directly linked to our mental and emotional health. As our body breaks down the gut microbiome, it releases by products called metabolites. These metabolites, along with the microbiota, communicate with the brain via the vagus nerve.
When we have a healthy selection of microbiota in our guts then we can send healthy and harmonious messages to our brain.
However, if our gut flora has more of imbalance and therefore is dominated by a higher selection of dysbiotic flora, it can send stress signals to the brain and lead to emotional and mood disorders such as anxiety, stress and depression.
Which in turn leads to more dysbiotic gut flora, and the cycle continues.
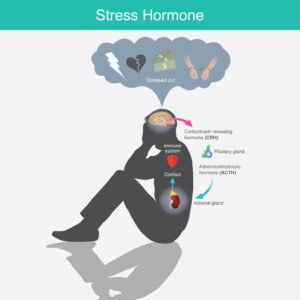
Long term stress and the HPA axis
The HPA axis involves the hypothalamus and the pituitary gland in the brain, as well as the adrenal glands. It is responsible for many processes in the body including digestion, sexuality, immune response and how you handle stress. It is also crucial for the coordination of your endocrine system with your nervous system, specifically your fight or flight response.
In short summary, when you perceive something to be a danger or a threat, action potentials in the brain trigger neuron’s in your hypothalamus to release a peptide hormone CRH. This hormone takes a short trip through the blood stream to the anterior pituitary gland and binds to a receptor on the target cell. This triggers the release of a hormone called ACTH which travels through the blood to your adrenal glands. This then triggers the release of a frenzy of different ‘freak-out’ compounds known as glucocorticoid and mineral corticoid hormones, simplified as cortisol. This activates the sympathetic nervous system which drives the body into what is known as the fight or flight response.
When your body is in the fight or flight response, a negative feedback loop is triggered in the hypothalamus to switch off the release of stress hormones and begins the slow process of down regulating the nervous system back into a calm parasympathetic state of rest and digest.
Long-term stress however, blocks this negative feedback loop reaction and switches off the HPA axis which in turn making it near impossible to self-regulate back to a calm state with an elevation of stress hormones circulating through your system.
This results in a reduction of brain derived neurotropic factor and serotonin and an increase in glutamtergic action in the amygdala which is associated with increased symptoms of anxiety and depression.
What this means for your gut microbiome
The impact of the excess stress hormones in your body dysregulates motility in your gut lining which in turn alters the gut microbiota composition.
This then decreases your gut barrier integrity, a protective epithelial lining, which leave the gut susceptible to invasive pathogenic bacteria and parasites.
Visceral hypersensitivity will also increase under this pressure thus resulting in higher levels of pain in your internal organs such as cramping, stomach aches and other internal sensitivities.
Under these conditions, your gut will continue to multiply the wrong kind of gut microbiota that are thriving in an unhealthy environment, as your gut continues to cater the perfect conditions for them to thrive.
Overall, this will all lead to a case of gut dysbiosis that will in turn increases the pro inflammatory cytokins which further releases more stress hormones, and again, the cycle continues.
Understanding the composition of your gut flora is essential for beginning your healing journey. Different microbiota will thrive in a variety of different environmental and dietary conditions, and sometimes its not just as easy as taking a dose of antibiotics and/or probiotics to restore your GIT back to health long term.
You can learn more about your gut microbiome by ordering a microbiome mapping test. Book an online Naturopathic consultation to start your healing process today.